TELUS eClaims allows allied health practitioners to submit claims to insurance companies on behalf of their clients at the point of care so they aren’t required to pay out of pocket. Practitioners were already very pleased with eClaims as a service but was due for a modernization.
As senior experience designer and project lead, my responsibilities included: Understanding the needs of health practitioners and administrators when it comes to their client’s benefit coverage and payment
Lead design - concept and wireframe development as well as visual design and asset design - for responsive portal redesign and new mobile app
Delivering an accessible solution to WCAG 2.1 AA standards - including guidance and support for development and QA
Collaborating with product team throughout needs discovery, design, development through to launch
Assisting with producing launch materials
If it isn’t broken, what is there to fix?
The eClaims service has been available to practitioners for 9 years. Regular check-ins with practitioners told us that, those who use it, are very satisfied with the service.
The real driver for the update was an outdated development stack, a dated visual design that no longer aligned with TELUS brand and no support for accessibility. This was an opportunity to redesign the portal to be flexible enough to support the product roadmap and evolution and support all of our users with an accessible solution.
Building a foundation that considers the future
The main objectives of the redesign
Build a foundation
Design with reusable components
Accessible for all
Designing building blocks
The portal redesign and its components would serve as a base for a design system for TELUS Health products. The design of eClaims (a service within the portal) is intended to be used as a template for other services as they’re updated or added.
A portal for everyone
The portal should be available to practitioners, regardless of ability. In order to communicate a consistent experience for all, we produced wireframes with instructions for assistive devices and screen readers for the developers.
For this project, the development team was new to accessibility so the UX designers provided a lot of additional markup, examples, training, and resources to get them started and get everyone on the same page.
Rethinking the task flow
The key task of submitting a claim for an existing client represented the majority of the activity in the portal. In its current state, the workflow was the same long form whether the client was there for the first time or a follow-up. We explored ways to make it even faster for claims to be submitted for existing clients.
Chunked information in the form for ease of navigating on smaller devices
By separating out the task flow of an existing client (the more common flow) and a new client we were able to find efficiencies.
Heading in the right direction? We made sure to check
Once we felt we had a clean, low-fidelity concept of the key task of claim submission, we scheduled some practitioners to see if they could intuitively and speedily walkthrough it. These sessions were done remotely using zoom conferencing and screen sharing.
Making claim submission a breeze
Submitting a claim took the forefront of the design, making it as quick and straightforward as possible to zip through claim submission and get a client processed. This could be done from the front desk or sitting next to a client in their home on their mobile device.
All claims
Notifications panel
Claim accepted
New claim workflow - Step 3: Service information
My account menu
Support panel
Not all practitioners have administrators with a waiting room
The majority of eClaims users are administrators who work primarily at a desk. However, some eClaims users are the practitioners themselves - they work independently, sometimes at multiple locations or they’re on the go traveling to clients’ homes.
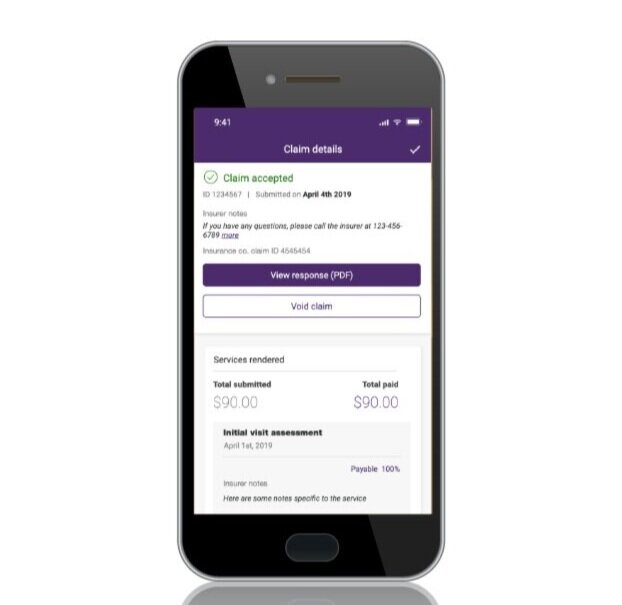
The mobile app was designed to support the needs of these users - The claim flow is made even more efficient by taking advantage of native features of the device.
Home
Claim accepted
Scan insurance card